Abstract
Background: Pediatric acute lymphoblastic leukemia (ALL) patients have excellent survival outcomes, yet remain at increased risk for impaired physical function due to multiple chemotherapy-associated conditions including myopathy, peripheral neuropathy, bone toxicities, and fatigue. While initiating physical therapy (PT) early in treatment is likely to improve physical function and overall health of children with ALL, there are no published recommendations to guide PT service delivery for this population. In fact, utilization of PT and factors associated with utilization during planned and unplanned hospitalizations are not known. We sought to determine patterns of inpatient PT utilization in pediatric ALL patients, and its association with patient and hospital factors.
Methods: Leveraging the Premier Healthcare Database, we conducted a cohort study that included participants hospitalized with ALL at 0-21 years of age from January 1, 2010 through March 31, 2017. Patients who underwent bone marrow transplant or had traumatic injuries unrelated to ALL therapy were excluded. The primary outcome was receipt of inpatient PT, identified by billing claims, within one year of first hospitalization. A multivariable logistic regression model was used to estimate odds ratios (OR) and 95% confidence intervals (CI) of sociodemographic and clinical variables associated with PT.
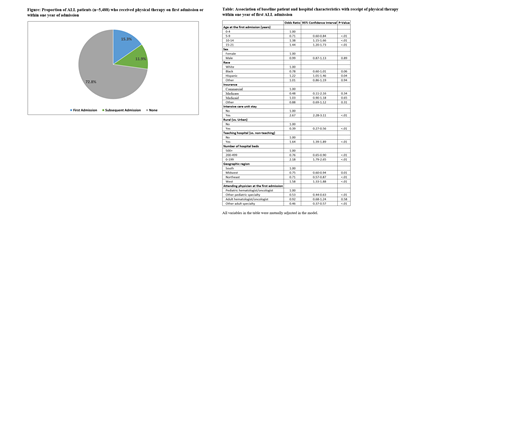
Results: Our cohort included 5,488 pediatric ALL patients admitted to 330 hospitals (42.3% female, 56.0% White, median age 7 years). Among these patients, 1,491 (27.2%) received PT within one year of their first admission, with 840 (15.3%) receiving PT during their first admission (Figure). For inpatient hospital stays in which participants received PT, the median length of stay was 9 (interquartile range [IQR] 4-18) days, and the median number of PT encounters per stay was 2 (IQR 1-4). Of 426 patients who had a diagnosis of peripheral neuropathy (n=334), myopathy (n=35), or avascular necrosis (n=74), 251(58.9%) received PT within a year of their first ALL admission.
Compared with patients 0-4 years old, those aged 5-9 were less likely to receive PT (OR=0.71, 95% CI: 0.60-0.84), while those aged 10-14 (OR=1.38, 95% CI: 1.15-1.66) and 15-21 (OR=1.44, 95% CI: 1.20-1.73) were more likely to receive PT (Table). Patient factors associated with receiving PT included Hispanic ethnicity (OR=1.22, 95% CI: 1.01-1.46) and a history of an intensive care unit stay (OR=2.67, 95% CI: 2.28-3.11). Patients at teaching hospitals (OR= 1.64, 95% CI 1.39-1.89) were more likely to receive PT than those at non-teaching hospitals, while patients at rural hospitals (OR=0.39, 95% CI: 0.27-0.56) were less likely to receive PT than those at urban hospitals. Compared to patients treated by a pediatric hematologist/oncologist, patients treated by a non-hematology/oncology pediatric (OR=0.53, 95% CI:0.44-0.63) or adult (OR=0.46, 95% CI:0.37-0.57) specialist were less likely to receive PT. PT utilization also varied significantly by geographic region, and hospital size, while patient sex and insurance coverage did not appear to impact PT utilization (Table).
Conclusions: Less than 30% of pediatric ALL patients receive inpatient PT within a year of their first hospitalization. Interventions to increase inpatient PT services to pediatric ALL patients and address disparities in PT utilization would be desirable to improve the physical function and long-term health of survivors.
Ma: Celgene/Bristol Myers Squibb: Consultancy, Research Funding.